In our efforts to provide insights to the healthcare industry from our 70,000 daily consumer/patient interactions, Carenet Health has new data to share from the frontlines of telehealth during the COVID-19 pandemic.
While virtual care usage is gaining unprecedented momentum among younger adults, our data shows that older and economically disadvantaged Americans may not be utilizing telehealth services with the same level of enthusiasm. The main takeaways of our recent telehealth visit analysis include:
- During a 10-day study period from March 8 to March 28, 2020, Americans under age 40 made up 35.6% of all Carenet’s telehealth visit triage cases and demonstrated a substantial increase from a pre-COVID-19 baseline of 98%.
- From our data, it appears that Medicare and Medicaid members are using telehealth services more now than in the recent past, but still less than the commercial/employer-sponsored health plan population.
- Medicaid’s low-income beneficiaries made up just 25% of Carenet’s telehealth triage cases during that same period.
- Patients of Medicare age accounted for 23.5% of Carenet’s telehealth cases.
While these findings aren’t all that surprising considering these vulnerable populations are typically harder to reach and more difficult to transition to virtual care, they highlight an opportunity for the industry to improve telehealth education and outreach to help Medicare and Medicaid beneficiaries utilize remote healthcare services—especially during a crisis like COVID-19.
COVID-19 hits older, income-disadvantaged Americans harder
Reports like this recent New York Times study suggest that Americans in higher income brackets who live in wealthier areas are more likely to be able to follow stay-at-home recommendations—effectively lowering their risk of contracting the COVID-19 virus. Other data, including this Kaiser Family Foundation report, indicates that people residing in areas of socioeconomic disparity are subject to stark disadvantages during the pandemic due to limited access to care and high rates of existing health problems.
Older adults over age 65 are known to be at higher risk for COVID-19 complications, and Medicare beneficiaries also stand to benefit most from virtual care during a time when leaving one’s home coincides with increased risks. Previous reports from Carenet Health telehealth nursing staff confirm that Medicare patients are typically more resistant to emergency department (ED) care.
The lower comparative telehealth usage of Medicaid and Medicare populations in our data is occurring despite recent government measures loosening restrictions on virtual care for those plan members and making telehealth services more accessible. Medicare’s telehealth coverage was expanded in mid-March, and state Medicaid programs were granted more flexibility to include telehealth visits and other services offered by telehealth companies.
More about the telehealth findings
The chart below clearly demonstrates shifts in telehealth patient case volume from March 8 to March 28. Here, we see a 98% spike for patients in their 30s, and a 79% spike for patients in their 20s.
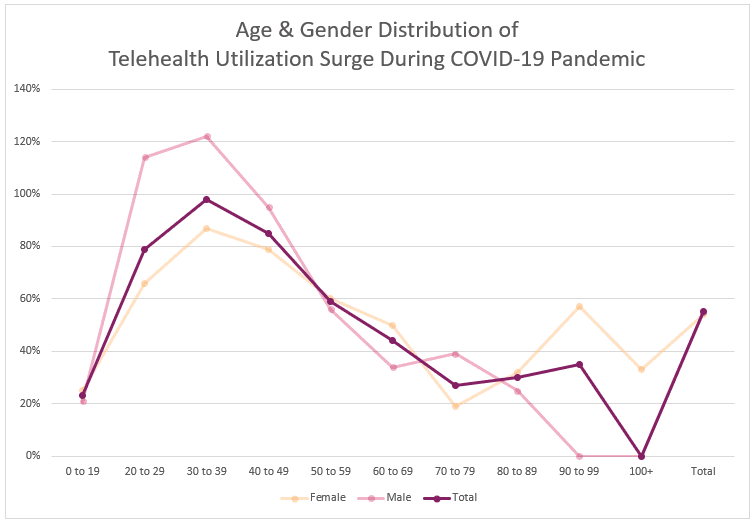
These findings align with the CDC’s recent income data showing that patients under age 50 accounted for 38% of U.S. COVID-19-related hospitalizations from February 12 to March 16.
The next chart illustrates how commercial/employer-sponsored plan members have increased their telehealth usage far beyond that of members who belong to Medicare or Medicaid plans.
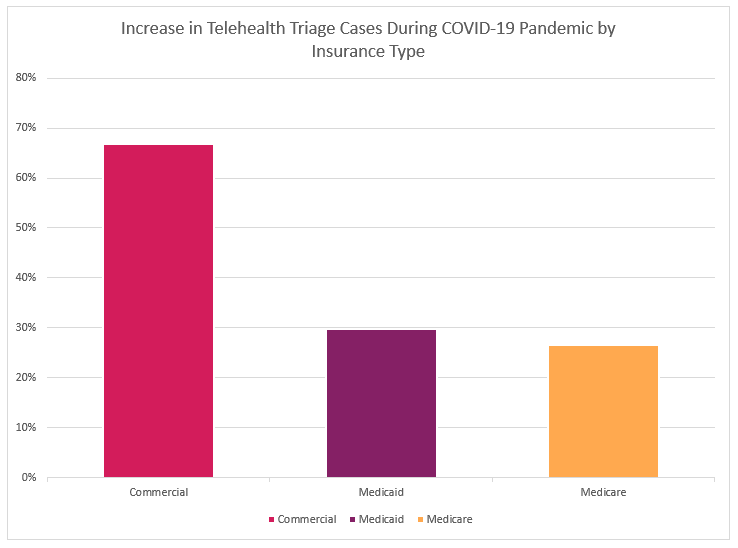
While many Medicare patients may be missing out on the benefits of telehealth due to simple lack of awareness, the low adoption numbers even in the face of recent government support suggest that older and lower-income Americans with COVID-19 symptoms may be more resistant to seeking out any type of care, including telehealth for coronavirus infection. On the other end of the spectrum, the big jump in people under age 30 who are using virtual care, despite the fact that they are far less likely to suffer severe effects, may reflect the younger segment’s high comfort level with technology.
All trends point to the need for managed care plans, Medicare Advantage plans and health systems to reach out to beneficiaries to improve their understanding of virtual care, educate them on how telehealth works, and communicate the benefits of remote services such as nurse advice line support for COVID-19 and mental health telehealth care.
Better telehealth engagement, better outcomes
While the importance of 24/7 telehealth services is recognized as an essential and valuable component of healthcare, there is room for opportunity to improve awareness and boost virtual care utilization. This is where cooperative, persistent outreach and education by industry partners—health plans, health systems, telehealth companies and others—can help by raising awareness and promoting widespread adoption of telehealth as an important supplement to traditional brick-and-mortar care.
As one of the top telehealth providers for COVID-19, Carenet is tracking the critical trends of coronavirus, and we’ll continue to share telehealth and healthcare engagement data and trends. Together, we can create and implement strategies to encourage telehealth understanding, usage and satisfaction—not only to help more patients get the care they need during a critical pandemic, but also to forge greater connection between patients and virtual care options for the future.