We’ve all heard the industry buzz around healthcare’s “new normal.” But in reality, a new normal doesn’t exist yet.
The pandemic continues to be anything but predictable. Community, regional and statewide outbreaks are in the news. Forecasting models depend on human behavior and the hoped-for success of public health initiatives. Patients’ post-discharge needs are evolving, and there is a growing list of long-term health effects that may drive continuing care management. And what happens when flu season hits, too?
All of this can leave health plans and other healthcare organizations preparing for fluctuating member engagement needs without a lot of confidence. Building out in-house staff readiness could be a significant waste of time and money if it ends up not being necessary.
Learning to share: The value of pooled engagement resources
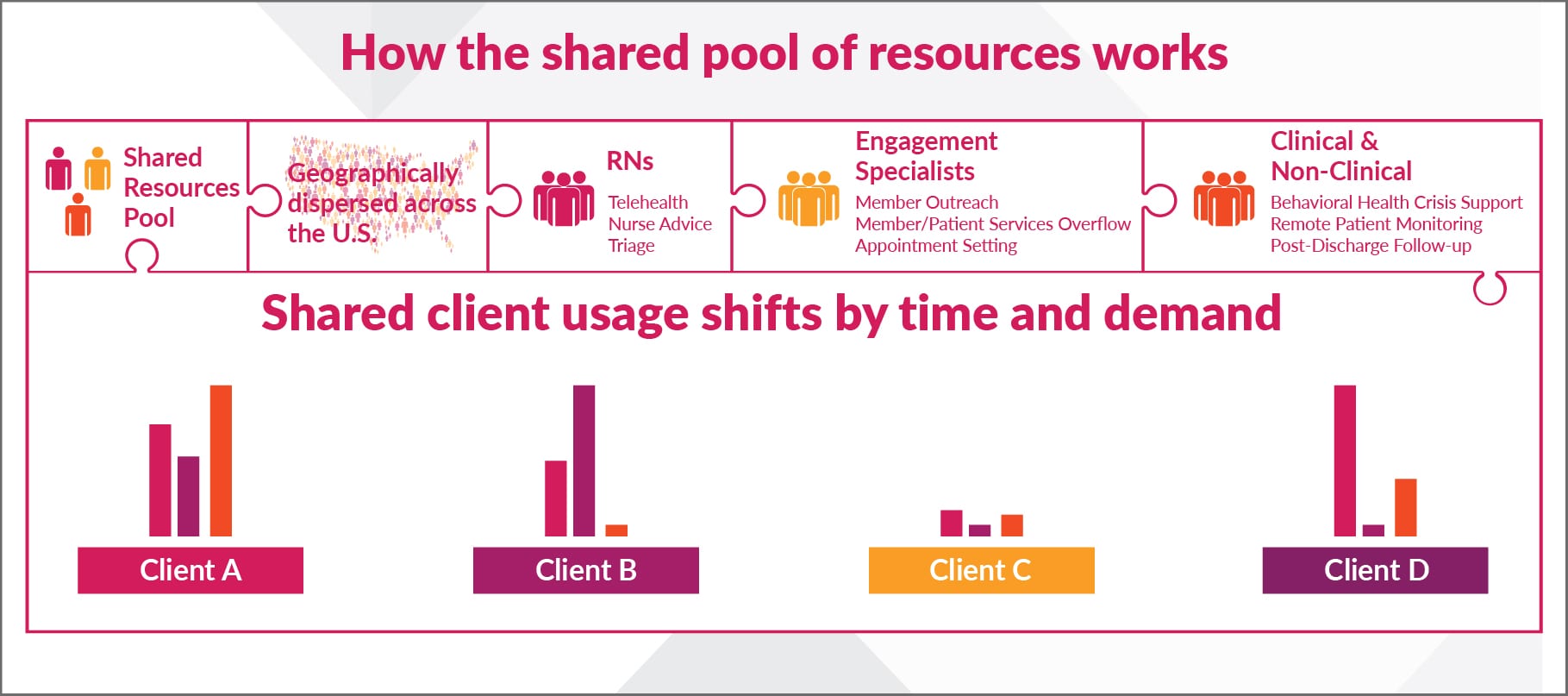
One solution for payers and providers is the use of an available, shared pool of non-clinical and clinical resources—whether it’s engagement specialists, member services professionals, registered nurses, care coordinators or health advocates—that can be tapped when demand increases.
It’s a flexible concept that means you typically pay for only what you need. Deploying just-in-time extra capacity via a shared pool allows you to adapt in real time to shifts in needs, and expensive dedicated teams don’t sit idle, waiting. Plus, a pool of shared professionals means you don’t have to support independent contractors or build a long-standing in-house team and support it over the long-term. (Shared services typically do require upfront contracts to secure your resources.)
Leveraging shared services, of course, is not a new concept. But it’s one that deserves a fresh look when current staffing is already near its limits.
Benefits of diving into the shared pool
A shared resource model works especially well when a trifecta of factors are in play: forecasting of demand and timing is difficult, you need to move quickly as needs change, and a cost-effective solution with low initial outlay is important.
Other key benefits can include:
- Exceeding consumer expectations 24/7. Members and patients in a crisis like a pandemic need help and answers, and they need them at 2 p.m. AND 2 a.m. Flexible, on-demand shared resources can deliver that around-the-clock service easier and more cost-effectively than one dedicated team with limited numbers of available hours. The importance of this benefit can’t be overstated in today’s world: A J.D. Power study found that U.S. health plan members haven’t felt supported by their insurers during the crisis. Sixty (60) percent said they weren’t contacted by their health plan with guidance or information related to COVID-19.
- Responding rapidly to emergent demands. A collective pool of resources is the epitome of flexibility. Availability of resources can be turned off and on with fluctuating requirements. (Geographic diversity in the talent pool is important here due to pandemic regional outbreaks.)
- Leveraging outside expertise. You may not have all of the in-house expertise, in the number of professionals needed, to meet engagement and telehealth demand in a crisis. A specialized healthcare shared service provider will. For instance, you may need member services professionals that also have in-clinic experience. Or you may need licensed behavioral health support that’s not available in your core skillsets.
- Enjoying industry-wide insights. Tapping into a provider of shared resources means you get insights on best practices from across the spectrum. This can leave your organization better prepared and informed. Testing of scripts and other engagement factors will also benefit all in the shared resources group.
- Freeing up your in-house teams. Because they aren’t frantically trying to handle sizable increases in member needs and calls, your professionals can focus their attention on fixed, not variable, needs.
Considerations when using shared engagement resources
Utilizing shared resource groups can have shortcomings that should also be considered. Addressing these upfront with your engagement and telehealth providers will be essential for success.
- Lack of special organizational knowledge in external teams. Organizations have distinct policies and cultures. A seamless consumer experience requires that the shared talent be trained in the specifics of the organizations using the resources. Staff should also be empowered to handle member needs and problem-solve without additional client intervention when possible.
- Quality monitoring and reporting. Even in a crisis, continuous quality monitoring and performance improvement should be a priority. Your metrics may be different than an external pool; you’ll need to address that and find solutions for reporting and evaluation, so you can ensure your members are getting the service they deserve.
- Technology integration. You will need time to connect your systems to those of the shared resources provider for a smooth consumer experience at launch. You may need devoted IT support on your end, at least for a little while, to make interoperability happen in a timely manner.
Ideas for ways to use shared engagement and telehealth resources
Many organizations think of using shared engagement resources for obvious needs such as customer service overflow or after-hours support. We’ve gathered some additional ideas for inspiration—ways you can use your portion of a talent pool to continue to increase care access and support for your members and patients:
- Nurse triage of member/patient calls for appropriate care direction (vital for symptomatic coronavirus patients)
- Telemedicine portal sign-ups and appointment setting
- COVID-19 testing results support and outreach
- Crisis or maintenance support for growing mental health needs
- Chronic disease engagement and care management
- Well-being check-ins (especially good for seniors)
- High-risk guidance and outreach (particularly COVID-19 related)
- Remote patient monitoring clinical support
- Support for COVID-19 at-home cases or after inpatient discharge
- Benefits navigation help for pandemic-impacted patients
- Virtual clinical support needs (important as employers implement return-to-work plans and employees need guidance)
- Transportation/in-person visit coordination for preventive care
- Medication refills and other treatment adherence support
- Closing gaps for proactive care, like mammograms and other cancer testing
It doesn’t have to be an either/or choice
Carenet Health offers a variety of engagement, telehealth, clinical support and advocacy delivery models, and we’ve found that no model is perfect in every situation. In fact, it often takes a combination of models to provide the levels of service today’s healthcare consumers need.
But with no crystal ball in sight, we’re encouraging health plans, health systems and provider-clinic networks to talk to us soon if you’re considering leveraging our limited amount of shared talent resources, or if you’d like to discuss setting up a dedicated clinical or non-clinical resource team.
___________
Learn more about our COVID-19 Shared Resources Support Center.



