America has the greatest healthcare in the world, but the costs – financial, operational and human – are too great to ignore. Together, we have the power to change it.
Carenet Health works with the nation’s leading providers and payers to identify opportunities and make these transformational changes. This resource center is here to help you do just that.
Helping executives surface the hidden costs stalling progress and the real path forward.
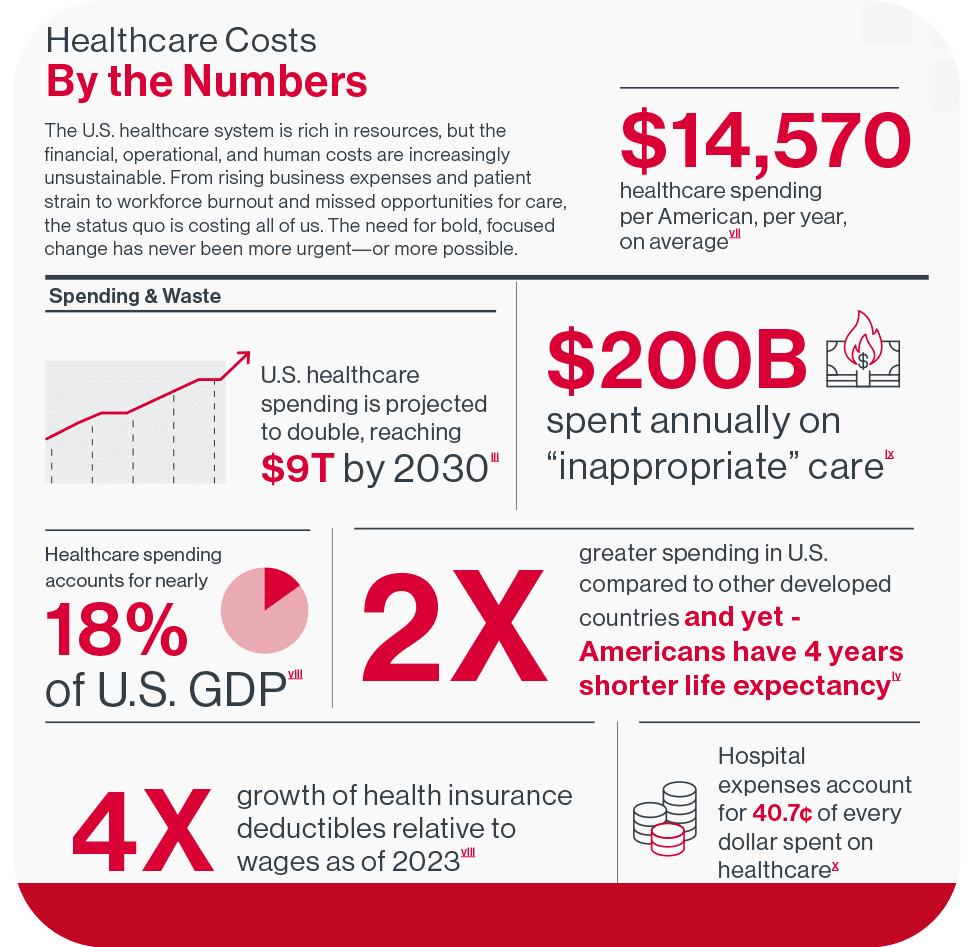
Financial, operational and human costs of healthcare in the U.S. are staggering. Here's a full picture of the toll they're taking.

Smart strategy, not blind adoption. See how leading health organizations are applying AI the right way

Specially curated list of current news impacting the business of healthcare and health outcomes today.

Check out some of the books Carenet's team is reading about leadership needed to Power Change in healthcare.

Panel discussion with healthcare leaders about using AI to reduce burnout, improve outcomes, and amplify human capabilities.
Missed out on HLTH25? Learn how we powered change at HLTH this year
Meet the organizations turning strategy into measurable outcomes. These case studies show how healthcare leaders are delivering better results through smarter orchestration of people, technology, and operations. This is what powering change looks like in the real world. Click the case study to download.
You’re managing budgets, launching initiatives, and adopting new technology. But what about the operational inefficiencies, trust erosion, and misaligned systems quietly draining your momentum? Healthcare executive Rhonda Gibler reveals why the most disruptive costs are the ones we’re not measuring—and how clarity is the key to transformation.

The primary causes include communication gaps between departments, manual processes that consume excessive staff time, fragmented data systems across multiple platforms, inefficient scheduling processes, and lack of standardized workflows. These issues compound to create delays, errors, and patient frustration throughout the care journey.
Healthcare organizations lose an average of $2.1 million annually to operational inefficiencies. On a national scale, inefficiencies cost the U.S. healthcare system over $935 billion per year through wasted resources, duplicate processes, administrative burden, and poor care coordination.
Patient complaints typically stem from long wait times, communication delays, repeated information requests, scheduling difficulties, and feeling like they’re navigating a complex system alone. When administrative processes are broken, patients lose confidence in the quality of care they’ll receive.
Common warning signs include staff spending excessive time on manual data entry, patients calling multiple times for simple requests, departments working in silos without shared information, high patient no-show rates, staff overtime due to process delays, and declining patient satisfaction scores.
Inefficiencies directly translate to patient frustration through longer wait times, communication breakdowns, scheduling problems, and the perception that their time isn’t valued. Research shows that operational problems are the leading cause of poor patient experience ratings.
Patient engagement drives measurable business outcomes: engaged patients are 3x more likely to adhere to treatment plans, generate 18% more revenue through referrals, and cost 30% less to serve due to improved communication and care coordination. It’s also directly linked to better health outcomes.
Patient satisfaction measures how happy patients are with their experience, while patient engagement measures how actively involved they are in their care. Satisfaction is reactive (how did we do?), while engagement is proactive (how involved is the patient in their health journey?).
While technology can accelerate improvements, many inefficiencies can be addressed through process standardization, staff training, improved communication protocols, and workflow optimization. However, sustainable, scalable solutions typically require some level of technology integration to maintain consistency and measure results.
The time for change is now. Read the Declaration every executive needs—surfacing the hidden costs stalling progress and the real path forward.