Smart Medicare Advantage (MA) plans are laser-focused on their CMS Stars patient experience scores. Typically, improving those experience scores comes down to at least these elements:
- Retaining your Medicare Advantage members and preventing member disenrollment
- Limiting and solving for member complaints and dissatisfaction
- Preemptively surveying and improving general satisfaction measured by the CAHPS survey
- Empowering your teams and providers to form nurturing relationships with members
Below, we break down four proactive strategies for MA plans to consider as they work on their improvement initiatives—including some strategies plans may not have considered yet.
Idea #1: Identify those members at risk for negative scores and offer them concierge-level service
The best way to begin neutralizing negative ratings is to target individual members who have indicated potential dissatisfaction with strategic communication. This population can be determined using analysis of data from ongoing NPS (net promoter score) surveying, narrow-network ZIP codes and official complaints.
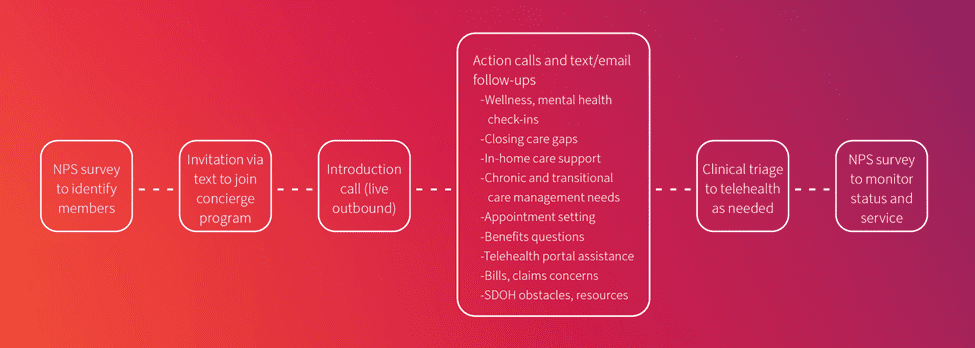
Once you’ve found your audience, consider offering these members a multichannel, concierge-level service program. The program should provide one-on-one connections that:
- Assist members with all of their healthcare and benefits problem-solving
- Actively listen to concerns
- Engage in a strategic cadence that ensures relationship- and trust-building
- Demonstrate empathy and the plan’s commitment to service
Here is an example of how that could look in practice:
For examples of advocacy programs in action, check out this blog post.
Idea #2: Adopt holistic engagement strategies that include mental health for all members
The pandemic has hit Americans’ mental health hard. With two-thirds of adults suffering from social isolation, issues like depression and anxiety are affecting people’s well-being in greater numbers than ever before. The mental health of your senior population affects a lot—physical health outcomes, quality of life … and satisfaction with your plan.
So, it makes sense that health plans that provide whole-person care with an increased focus on mental health may achieve better outcomes and higher Star ratings. At Carenet Health, we recommend developing programs that target both mental health crises and maintenance support, as well as help members access local social services.
Another important step should be educating your members about the resources you offer, whether that’s 24/7 nurse triage or virtual counseling sessions. Be sure to clearly communicate the costs associated with the support offered and any self-help tools members can use. Remember to check in on members periodically.
Telehealth, including virtual behavioral health care, can impact a number of Star ratings, as well. And chances are, it’s being underused as an improvement tool by your Medicare Advantage plan. Read more about that here.
Idea #3: Pay more attention to getting better at provider-payer engagement
The fact remains that a majority of a Medicare Advantage plan’s Star ratings can be linked to what happens or doesn’t happen between patients and providers. Health plans should have a process in place to reach out to providers to establish connections, coordinate care and seamlessly manage referrals.
But importantly, beyond that, does your organization have a plan to measure the success of that process? Can you identify, in near-real time, areas that need improvement? Can you implement optimizations quickly?
In the past, provider-payer engagement hasn’t had the same headline appeal as direct-to-consumer engagement, with all its bells and whistles. But it deserves a strategy for continuous improvement.
Idea #4: Take member surveying to the next level
Year-round, frequent member surveys can help your plan measure patient experiences and inform next steps for addressing any issues the surveys may reveal. Now is a good time to unpack and review your:
- Surveying tactics,
- Channels,
- Scripts, and
- Partners
—and find areas that could use a refresh.
Just one example: What happens during a surveying call when a member has a complaint? Is that member immediately warm-transferred to someone who can address their concern? The same question should be asked when you’re using a portal survey tool or a survey sent via text.
Another way to build on a frequent surveying strategy is to develop member sentiment analysis that correlates findings to specific provider groups, demographic groups and/or geographic areas—so that you can identify where your best opportunities lie in improving member satisfaction and experience.
—
If you’d like more ideas and strategy planning templates for designing your Medicare Advantage member satisfaction improvement initiatives, download our Stars Planning Toolkit.


