The Importance of a Successful Healthcare Member Engagement Strategy
John Erwin, CEO of Carenet, says the executives he speaks with across the industry often focus on consumer outreach when they strategize about engagement. “There is a heightened emphasis on engagement as all of the ways an organization communicates with members and patients,” he says. “For example, they may say, ‘we touch each of our members 100 times per year,’ and this number includes all the forms of outreach with members.” John says the elements that are often missing in that dialogue are: Did you really make a connection with a member? Did your outreach lead to them taking a specific action? The other perspective also growing in significance is engagement as customer service and member support. “Many health plans may look at engagement as purely contextual,” says Steve Harstad, Chief Strategy Officer at Carenet. For instance, they might track:- Digital engagement: Did members log in, take action with an app, or return to a site or app?
- Wellness engagement: Did members enroll in a program? How many program steps did they take? How many coach/RN calls did they complete?
- Quality engagement: Which care gaps were closed? What was the level of patient adherence? What was the number of care management program enrollments?
What health plan member engagement isn’t
Sometimes it’s easier to figure out what something is by understanding what it isn’t. When we asked our leadership team to think about what member engagement should not be about, they provided some insights based on what they’ve seen in the marketplace. “Engagement does not mean texting or emailing or web chat. Those are tactics that help you succeed in engagement, but engagement is much more than tactics,” says Jim Caswell, Director of Business Development. David Dreggors, Vice President of Business Development, agrees. “It’s not simply reaching a member’s phone or email inbox or leaving a message without actually interacting with the member,” he says. It also isn’t about how being heavy-handed in asking members to take action or overwhelming them with unwanted contact. It’s a delicate balance of touchpoints, encouragement and action.
Going beyond outreach to impacts
There’s a clear thread here. Health plans must begin measuring more than merely outreach volume. They must measure whether a valuable and meaningful conversation happened, and whether the service or support they offered made a difference to the member in terms of helping them more easily achieve a successful health outcome. Arianna Brazelton, Senior Client Relationship Manager, agrees with this perspective, saying, “Engagement is really all about driving members’ utilization of the plan’s benefit tools and services in ways that empower members to achieve better health.”So, what do health plan members want? Let’s take a look.
Perhaps most important in informing an engagement definition, health plans need to take note of what their members say they want from insurers—and then deliver on those desires. So, what do members want? Let’s take a look.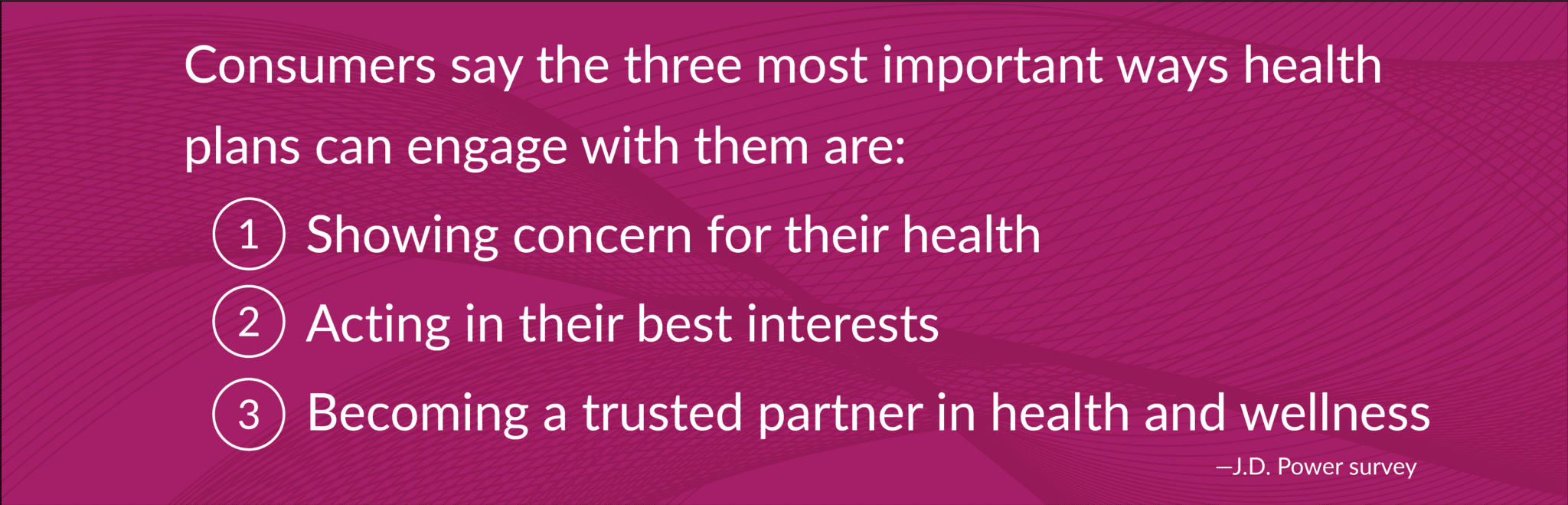
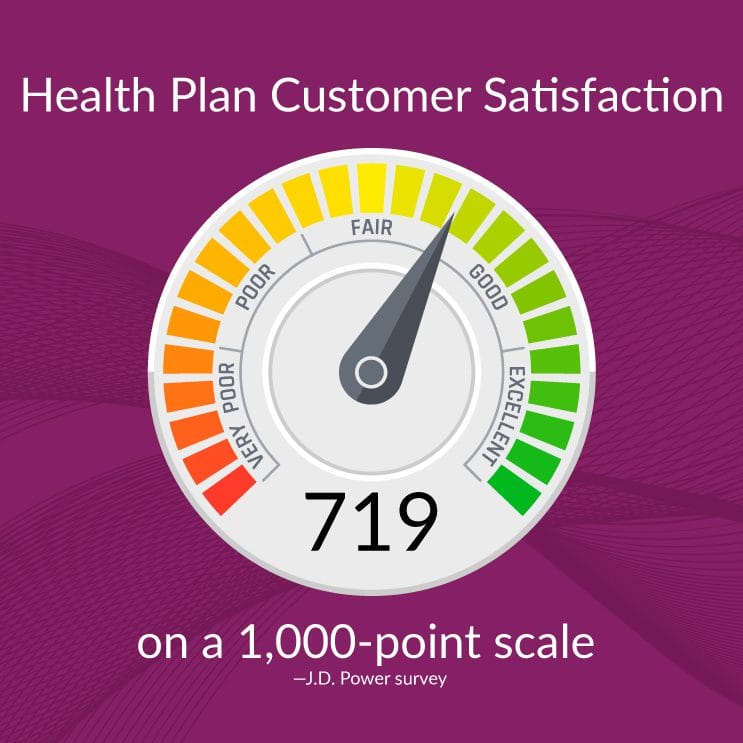
A Verint research report, Experience Index: Health Insurance, also found that members considered factors like the value they were getting from their health plan (premium cost, level and thoroughness of coverage) as the most important factor of their overall satisfaction.
The second and third most important factors were the enrollment experience (number of plan choices and options, ease of enrollment) and the health plan’s services (availability when needed, responsive to needs, ability to answer questions).
The level of member satisfaction is important for many reasons, but especially for becoming a trusted partner. Verint’s research showed that satisfied members were also more likely to trust their health insurer.
Delivering customer-centric engagement requires a much different and more holistic approach than simply sending an email or responding to a web chat.
From buzzword to success in the real world
Targeted consumer outreach can help individuals make and keep appointments, including visits for vaccinations, preventative care and chronic disease management. And beyond that, targeted outreach should create a springboard to trust and connection.
Engagement done right will require a hard look at a health plan’s brand promise and the specific member populations served. A Medicare audience might require a different approach than a commercial audience. Medicaid might be different by state or region or between urban versus rural.
Yet there are some factors that tend to be universal—factors that health plans should consider incorporating into member engagement efforts. These include:
- Leveraging consumer data to help guarantee that information is personal, relevant, and timely
- Providing focused, conversational messaging to move consumers to action and demonstrate you truly care
- Deploying a multi-channel, multi-touch strategy built on members’ communication preferences that emphasizes awareness, education and scheduling convenience
- Offering a single, simple point of contact (preferably on-demand, 24/7) to make it easy for members to gain access to information and answers
- Providing cost-savings and incentive programs that educate members on what their benefits are and help them use those benefits to ensure they get the most from their plan.
Taking payer member engagement to the next level
The definition of health plan member engagement may be fluid, but one factor won’t likely change: Success requires helping members take their next-best step to health and wellness, looking beyond conventional connection metrics, and communicating with members on a deeper, more personal level—both when they contact you, and when you contact them.
Perhaps health plan member engagement, while multi-layered, actually comes down to a single point. As Lisa Policano, Director of Business Solutions at Carenet, says, “Sometimes, engagement can just mean doing everything in your power to build really strong relationships that result in empowered, action-taking, satisfied members.”
Ready to continue the discussion with our experts? Contact us today.



