
Carenet’s consumer health report reveals opportunities for insurance plans to improve the member experience. Part 1 of the blog series on the report explored what drives members’ trust, pain points related to phone support, and members’ preferences for using technology to manage their care.
Download the full report here.
Part 2 will examine factors that drive member satisfaction and loyalty, perceptions of customer support and service, and steps that insurers can take to better educate members about their benefits. Based on a third-party survey of more than 1,200 adult respondents in the United States who have health insurance, the report provides an in-depth overview on how members really feel about their insurance plans.

Working with more than 100 payers nationwide, Carenet’s proven solutions help insurance plans boost member loyalty, increase access to care, improve customer support systems, and provide ongoing education to members about the benefits available to them.
Download the full report here.
How feeling cared for correlates with brand loyalty
Most Medicare and Medicaid members said their insurance company cares about their health and well-being, compared with a lower percentage of those with commercial plans who felt the same way. The perception of feeling cared for directly correlates with brand loyalty, as over 90% of Medicare members indicated they are either very loyal or moderately loyal to their insurance company. For instance, one of our case studies shows how Carenet elevated Medicare member engagement and drove $700 million in revenue for a large Medicare Advantage plan.
The insurer-member relationship is also fostered by communication, as 70.6% of respondents who indicated they are very loyal to their insurers said they receive regular correspondence from their insurance company. This finding highlights the importance of how engaging members through communication directly impacts their loyalty to a health insurer. Carenet has proven experience helping health plans to successfully leverage communication and awareness to drive member loyalty through multifaceted initiatives.
Respondents who said they feel that their insurer cares about their health and wellbeing:
- Medicare members (78.9%)
- Medicaid members (74.1%)
- Commercially insured (60.5%)
Over 90% of surveyed Medicare members said they are loyal to their insurance company.
Continually improve the customer support experience
When asked how their telephone customer support experience could be improved, shorter wait times and faster issue resolution were the two most-cited issues that respondents said would have a positive impact on their experience.

These findings point to the need for health plans to continually measure the metrics of their telephone customer support systems. Health plans that are working to improve the member experience turn to Carenet to strengthen their telephone customer support systems.
Establishing service-level agreements to support system metrics and benchmark performance against other plans and industries can help facilitate consistent performance and highlight improvements to address members’ pain points.
Factors that would improve the customer experience, according to respondents who ranked health insurers unfavorably for phone support:

- Shorter wait times (52.0%)
- Faster issue resolution (45.7%)
- Not having to repeat why they called after being transferred (43.3%)
- Eliminating language barriers (34.7%)
Health plans must continually measure the metrics of their telephone customer support systems.
Member benefit awareness is paramount
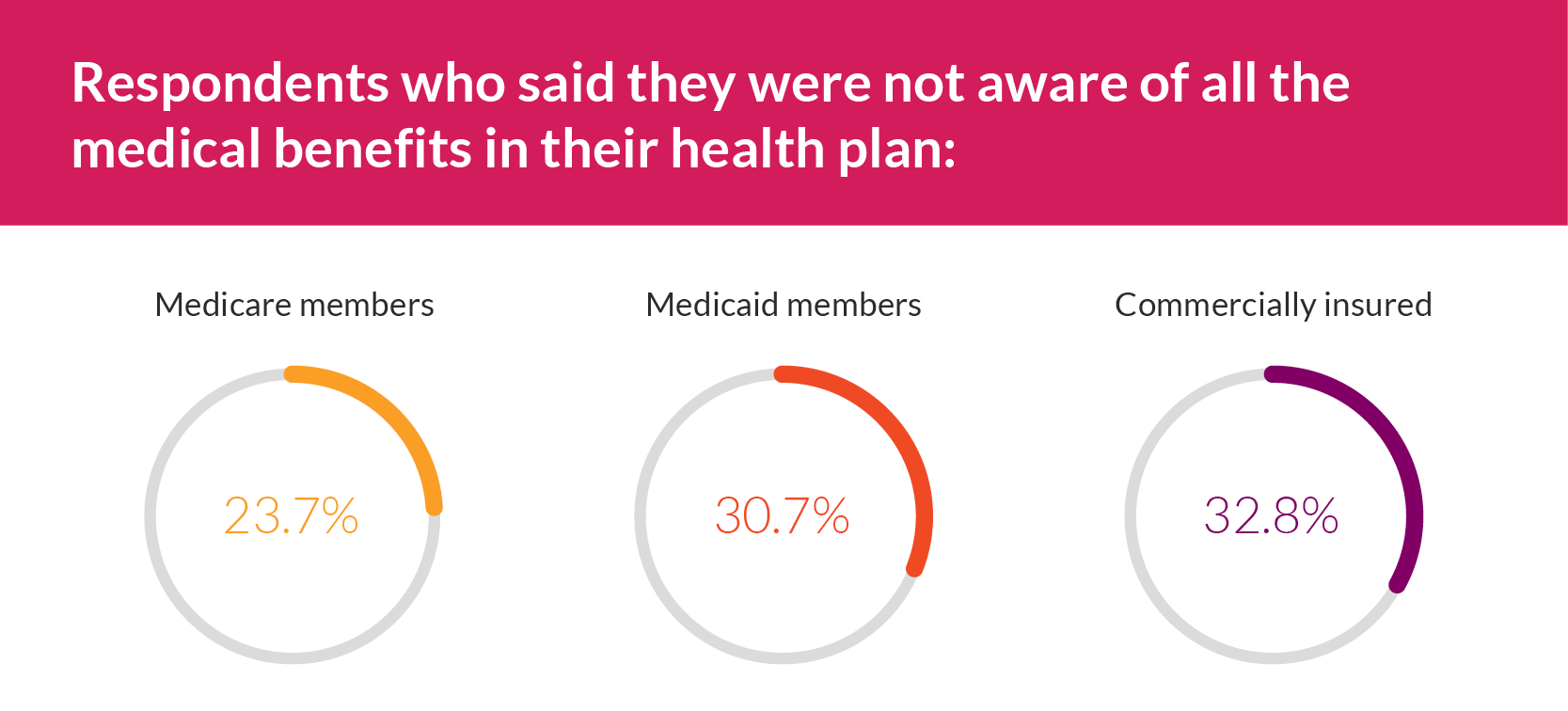
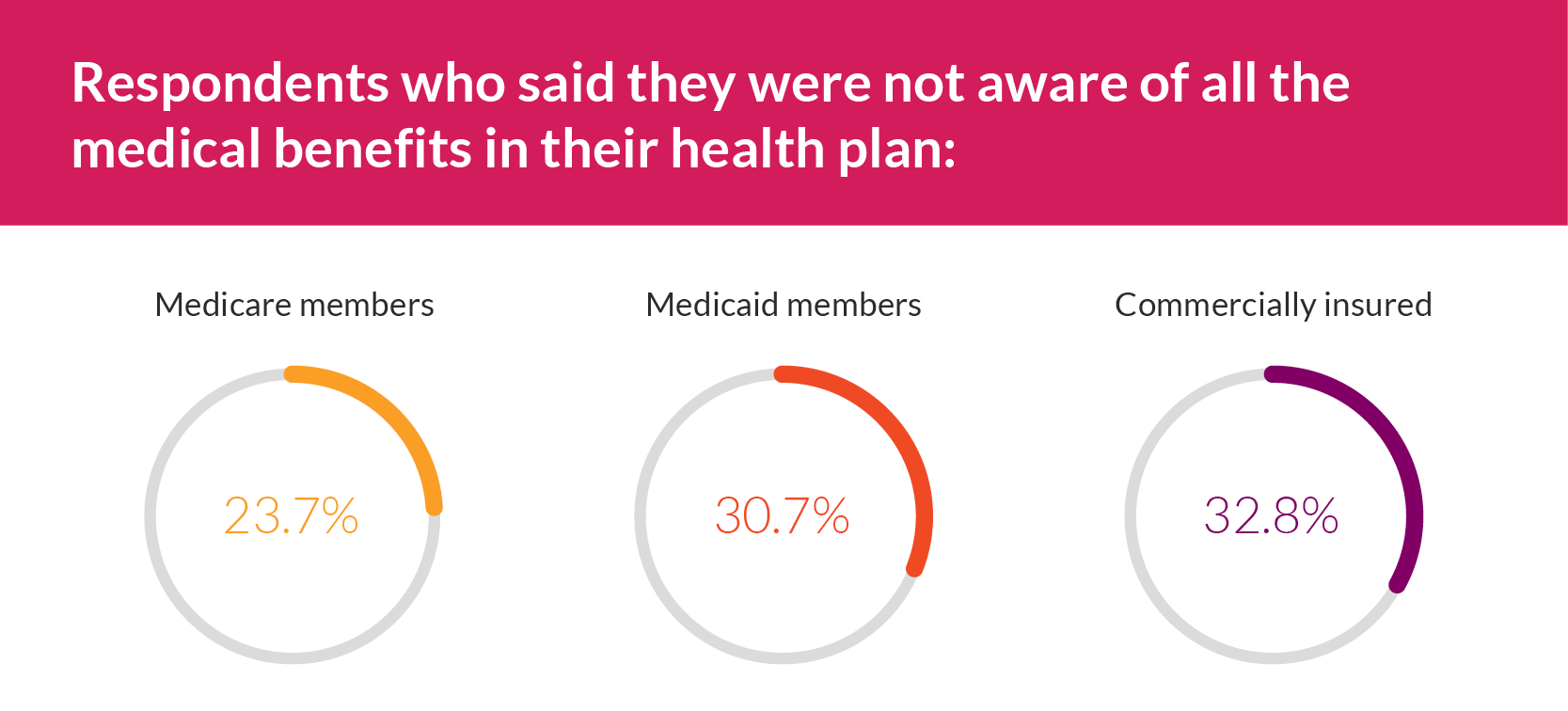
While most respondents indicated they were aware of all the benefits their health plan offers, nearly one-third said they were not. Medicare members had the lowest percentage of respondents who said they were not aware of all the healthcare benefits in their plan. This finding reflects a pattern in our survey data that points to Medicare members being more educated about their insurance coverage than Medicaid and commercial plan members.
Most respondents (71.3%) rated their level of understanding of their benefits as either excellent or good, while more than one-quarter said that their level of understanding was either fair or poor. This is not only disadvantageous to members, but it can also mean that an insurer’s customer service resources could be stretched thin if agents spend disproportionate time explaining benefits to individuals versus resolving members’ issues.
Respondents who said they were not aware of all the medical benefits in their health plan:
- Medicare members (23.7%)
- Medicaid members (30.7%)
- Commercially insured (32.8%)
Nearly one-third of all respondents said they are NOT aware of all the benefits of their health plan.
Carenet is using the findings of the Healthcare Consumer Insights: Understanding the Health Insurance Member Experience report to elevate our exceptional payer solutions and improve member experiences.
To learn more about the research findings, visit here.
Carenet leverages insights from consumer surveys and member experiences to improve the health insurance consumer experience. To learn more about Carenet’s member engagement solutions for health plans, visit www.carenethealth.com and stay tuned for future blogs highlighting insights from our report, Healthcare Consumer Insights: Understanding the Health of the Insurance Member Experience.


